Tricompartmental osteoarthritis is the most complex type of knee osteoarthritis and affects only 1.5% of knee osteoarthritis sufferers. Fortunately, there are ways to address it and manage it, including at least one non-invasive method which will be discussed later.
Understanding arthritis and osteoarthritis
You probably know a number of people who suffer from, what they call, “bone-on-bone” knee pain. This means the bones are rubbing together without the smooth protective layer of cartilage protecting them.
And it’s very prevalent.
Osteoarthritis (OA) is the most common type of arthritis, and affects more than 32.5 million people in the US alone. Knee OA can cause a lot of pain and stiffness affecting the quality of life to a lot of people. It is also becoming more prevalent and the people suffering from Knee OA has DOUBLED since 70 years ago.
And, as noted, while tricompartmental osteoarthritis is the least prevalent form of knee osteoarthritis, it is also the most complex.
What is tricompartmental osteoarthritis?
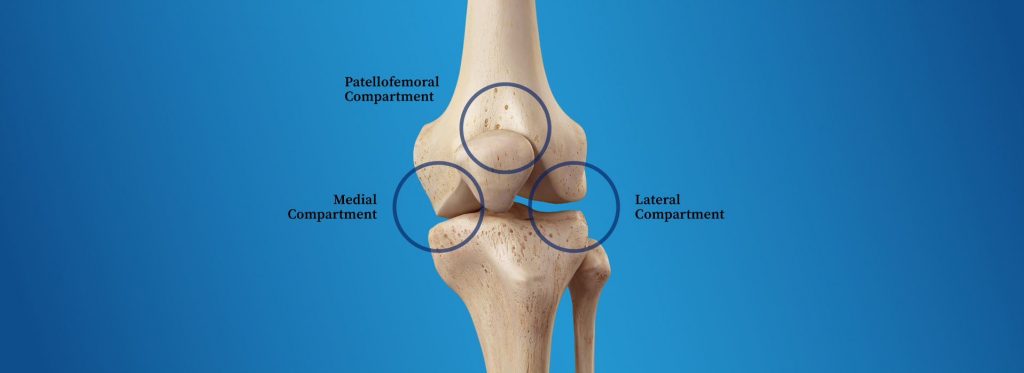
To understand tricompartmental osteoarthritis, it is important to understand that there are three parts — i.e. compartments — of the knee. Osteoarthritis can affect any one of the compartments, but if you have osteoarthritis in ALL THREE compartments, that’s tri-compartmental. Hence the name, “tricompartmental osteoarthritis.”
Try to imagine the cartilage of the knee joint being so deteriorated that the deterioration is in all three parts, that’s what we’re talking about. And although, such a thing may seem impossible to live a normal life with, there are people who are able to. The key is having good walking mechanics, or “gait” which is something that can be improved with the right kind of treatment program.
How does tricompartmental osteoarthritis affect the knee?
The knee is a hinge joint that allows your leg to move back and forth, but it doesn’t move much from side to side. Four bones meet at the knee joint: the femur (or thigh bone), the tibia (or shin bone), the patella (or kneecap), and the fibula (or calf bone). The tibia and fibula connect below the knee joint, the femur connects above the knee joint, and the patella rests on the femur and the connecting cartilage.
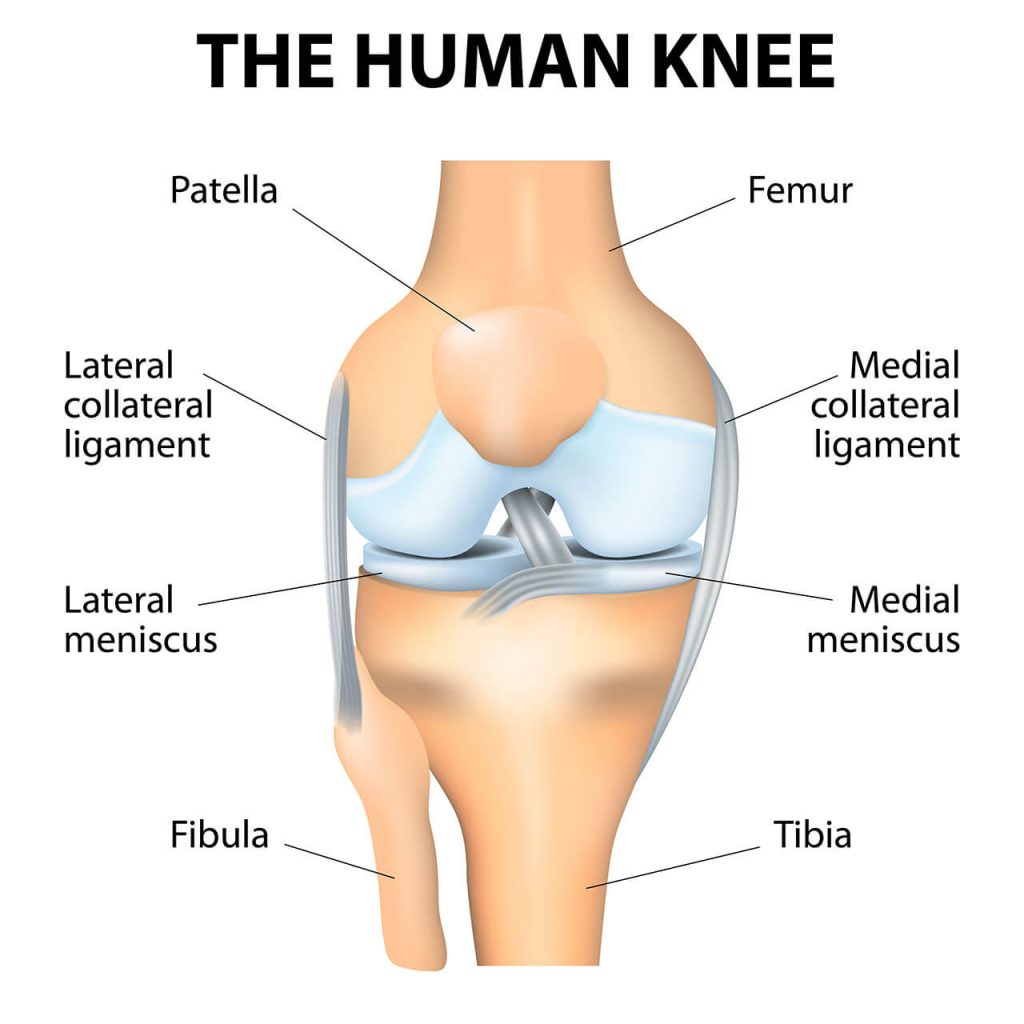
In addition to these bones, the knee is also made up of cartilage, ligaments, tendons, and more, with all of these parts working together to keep the knee stable and flexible. As you can tell, it’s a very complicated joint with a lot of moving parts that need to work together.
Tricompartmental osteoarthritis occurs when you lose protective cartilage from all of the areas where the bones meet the knee joint, damaging your biomechanics and throwing off your gait. These areas are called compartments. There are 3 compartments:
- The patellofemoral compartment is in the front of the knee where the kneecap and thigh bone are.
- The medial compartment refers to the inside compartment of the knee joint.
- The lateral compartment refers to the outer compartment of the knee.
Osteoarthritis can affect any of these compartments, or any combination of them, although it’s most common in the medial (inner) compartment. When one compartment of the knee is affected, this is called unicompartmental OA. When all 3 compartments of the knee are affected, this is tricompartmental osteoarthritis.
What are the symptoms of tricompartmental osteoarthritis?
The symptoms of tricompartmental osteoarthritis are similar to those of other forms of osteoarthritis, but this time they affect all three compartments of the knee. Pain is the main symptom, as well as:
- Knee pain that may be more severe during or immediately following activity
- Joint stiffness that may be more severe after sitting or first thing in the morning
- Joint tenderness
- Impaired range of motion—you may not be able to fully extend the knee
- Grating or grinding sensation in the knee, also called crepitus
- Popping or clicking noise when bending or extending the knee
- Development of bone spurs, or lumps, on the knee bones
- Knee inflammation due to synovitis
- Joint locking, weakness, or buckling
- Gait changes, for example, bow-legged or knock-knees
- Impaired mobility and stability
Often, patients only seek medical attention when their knee pain becomes acute, but they’ve generally already experienced symptoms for a while before this point. In the earlier stages of tricompartmental OA, symptoms will likely be mild and intermittent. However, as cartilage degeneration progresses, symptoms will become more frequent and severe.
What are the risk factors for tricompartmental osteoarthritis?
There are many issues that can increase your risk of developing tricompartmental osteoarthritis, or any kind of knee OA for that matter. Even if you have already developed tricompartmental osteoarthritis, you can still take steps to lessen the pain and improve your function. These are the risk factors to watch out for:
Obesity
The connection between obesity and joint pain has been linked through multiple clinical studies. And it’s also been shown that losing weight can slow the deterioration of cartilage.
This means that losing weight can be a good step in the right direction.
Posture
Your posture can contribute to the development of knee OA. While good posture helps muscles and bones minimize the stress on your joints, bad posture does the opposite. By improving how you stand, sit, and move, you may be able to slow the progress of the disease.
Gait (the way you walk)
As you know, your knee is involved in many movements, including:
- Kneeling
- Squatting
- Lifting
- Climbing stairs
- Walking or running
If your gait, or the way you walk, is not smooth it causes you to have bad biomechanics and your knee joint won’t move smoothly against the other components of your knee. Once your knee is even slightly out of position, you can end up misaligning it even more as time goes on. This causes other bones and tendons to rub against the joint, causing it to degenerate faster and placing strain on the misaligned ligaments and tendons, which disrupts your biomechanics even more, and so the vicious cycle continues.
Genetics
Family history, or genetics, can contribute to your chances of developing tricompartmental osteoarthritis. While scientists don’t fully understand how an elevated risk of developing OA is passed on, it’s likely that if you have several family members that have OA, there is a higher chance that you also are at risk. So, although you can’t change your genetic makeup, at least if you know that you have a family history of OA you can look out for the earliest signs and start treating it before it develops into a serious condition.
Gender
Knee OA, including tricompartmental OA, affects women more than men. Until around the age of 45, rates are similar, but this changes with more advanced age. In addition, women have been found to wait longer before seeking treatment, or to have more debilitating pain when they seek medical attention.
Age
Cartilage loss is associated with aging, so it’s not surprising that knee OA becomes more common as you get older. That is one reason why it is preferable to identify the disease early on in order to address it during earlier stages.
How is tricompartmental osteoarthritis diagnosed?
When you go to your doctor with knee pain, they’ll first ask about your symptoms, which will help them decide if you meet the criteria for knee OA. Your symptoms will also guide your physician to identify which compartments of the knee are affected.
You may be referred for an x-ray or other medical imaging process to confirm bone loss or cartilage damage. Imaging is a more precise method of diagnosing tricompartmental osteoarthritis. While early on in the disease’s progression, visual changes may not be obvious, as OA worsens, there will be evidence of osteophytes and narrowing of the joint space.
What a tricompartmental osteoarthritis diagnosis doesn’t tell you
It’s important to realize that once you have a diagnosis of tricompartmental osteoarthritis based on x-rays or medical imaging, that only tells a part of the story. It tells you how your cartilage and bones have been affected and how they look. The other part of the story relates to the way you walk — or your gait. A gait analysis can help a trained professional determine how the way you move can be adjusted in order to improve your situation. This is the idea behind AposHealth®.
Treating tricompartmental osteoarthritis
Unfortunately, there’s currently no way to cure osteoarthritis, although researchers are currently testing novel approaches to joint pain treatment. But there are ways to ease the pain, slow down progression, and improve knee function so that you can regain your mobility.
Weight loss
Managing one’s weight can help reduce strain on the knees, and maintaining a healthy weight and balanced diet are also important for overall health and wellness. Losing weight can also improve biomechanics, plus recent research discovered that weight loss has a protective effect on knee cartilage.
Exercise and physical therapy
Careful exercise can strengthen the muscles around the knee for better stability and mobility. Some examples include aquatic exercise and stretching. Physical therapy may also be prescribed to improve flexibility and strength and to improve gait.
Support aids
Supportive aids such as walkers, braces, splints, or therapeutic tape may help reduce pain. But not every support is suitable for tricompartmental osteoarthritis, so it’s important to ensure that you’re getting the right device for your needs.
AposHealth®

AposHealth® has been shown to shift the center of pressure away from the painful area, inducing new motor learning pattens of standing and moving, towards the desired neuromuscular gait pattern. Numerous clinical studies have shown that by using AposHealth® to adjust one’s gait brings with it significant improvements of function and temporary pain relief. The satisfaction rate of patients with knee osteoarthritis treated with AposHealth® is 96%41.
Over the counter symptom relief
Many knee OA sufferers find temporary relief from symptoms by using heat and ice packs, or over-the-counter non-steroidal anti-inflammatory drugs (NSAIDs). These may be effective at earlier stages of the disease, but as the pain worsens, they may not be enough. They only target the symptoms of tricompartmental OA, but not the causes of the problem and does not change the gait.
Prescription medication

In the later stages of knee OA, your physician may prescribe oral painkillers and anti-inflammatories, or corticosteroid injections. However, these medications do carry risks. NSAIDs can be dangerous for older users or people with high blood pressure, and opioid pain relievers are habit-forming. Before taking any medication, it’s important to discuss the risks with your physician.
Knee replacement surgery
If your pain and loss of mobility are so severe that they are impacting your quality of life, your physician may recommend total knee replacement surgery. This involves removing the damaged bone and cartilage, and replacing them with an artificial knee joint.
According to the American Academy of Orthopaedic Surgeons, up to 90% of patients who have undergone total knee replacement surgery report reduction in pain levels and increased mobility. However, this is a serious procedure that requires months of recovery. You will likely need physical therapy, follow-up appointments, and medication. Surgery should be considered a final option when other non-invasive modalities have not been effective.
Summary: Tricompartmental knee OA can affect your life, but there is still hope
Knee OA is a highly prevalent disease that affects millions of Americans and costs billions of dollars in medical and peripheral costs every year. As people get older, their risk of developing knee OA in general, and tricompartmental osteoarthritis in particular, increases. With no full cure for tricompartmental OA, it’s preferable to identify it early on so that progression can be slowed and pain eased, helping maintain your mobility and independence for longer.


